(P 218) SEX DIFFERENCES IN THE ASSOCIATION OF ALCOHOL INTAKE WITH THE RISK OF SOFT-TISSUE SARCOMA: A NATIONWIDE POPULATION-BASED RETROSPECTIVE COHORT STUDY

Min Wook Joo, MD, PhD
Associate Professor
The Catholic University of Korea
Seoul, Seoul-t'ukpyolsi, Republic of Korea- YC
Yoon Joo Cho, M.D., Ph.D.
The Catholic University of Korea
Seoul, Seoul-t'ukpyolsi, Republic of Korea
Author(s)
Co-Author(s)
Objective: Soft-tissue sarcoma (STS) is a rare and often deadly disease, constituting a group of diverse malignant neoplasms of mesenchymal origin. Notably, with the declining birth rate and increasing aging population, the incidence of STS has been increasing while that of bone sarcoma has been decreasing. Soft-tissue sarcoma may be associated with effects of demographic, environmental, and lifestyle factors although most cases are believed to be sporadic and some are caused with radiotherapy, inherited cancer syndrome, and damaged lymph system. Overweight and obesity, alcohol, tobacco, maternal late first pregnancy, viral infections, and chemical exposure (Agent Orange, chlorophenol, and cutting oil) may contribute to the risk of STS. However, evidence to draw conclusions on the risk factors is limited.
Worldwide, alcohol consumption stands as a leading risk factor for oncogenesis and related deaths. Ethanol in alcoholic beverages and acetaldehyde, its major metabolite, are categorized as group 1 (carcinogenic to humans) by the International Agency for Research on Cancer. Nevertheless, global per-capita alcohol consumption has been increasing, and the upward trend poses a potential risk of escalating the overall burden of cancers. In particular, the Korea National Health and Nutrition Examination Survey reported that the prevalence of high-risk drinking, defined as the proportion of people aged ≥19 years who drink ≥2 times per week and consume a large amount of alcohol each time (an average of ≥7 glasses for male and ≥5 glasses for female per episode) was 3.4% in 2005 and 8.4% in 2018 among women, implying a pronounced rising trend.
Therefore, alcohol consumption might be a risk factor for STS. We conducted a population-based study using the nationwide claims data to explore the association between alcohol consumption and STS risk, and its differences between sexes, focusing on alcohol consumption and drinking frequency.
Methods: This was a retrospective population-based cohort study. Using the National Health Insurance Service (NHIS) database, which represents the South Korean population, we analyzed 4.2 million Korean adults aged 20 years of age and older. In South Korea, NHIS serves as a single health insurance provider to all Korean citizens and provides biannual regular free health checkups. This database includes demographic, socioeconomic, health checkups, and claims data of all insured Korean people. The checkup programs include data for medical history, family history, height, weight, waist circumference, blood pressure, laboratory tests, hearing and visual checkups. Also, in 2009, according to the activation of the Basic Act on Health Examination, social behavior surveys including smoking, alcohol consumption, and exercise were added. Therefore, we included individuals who underwent NHIS health checkups between January 2009, and December 2009, and tracked them until December 2020 to identify the incident of STS. The participation rate for NHIS health checkups in the index year 2009 was 67%.
We initially screened 4,234,415 participants who were aged 20 years and older and underwent health checkups in 2009. Among them, 286,384 individuals were excluded due to incomplete data, and 198 patients who were already diagnosed with STS before the index year were also excluded. In addition, to clarify causality, we excluded 10,088 participants who died or developed STS in the index year. Finally, we included 3,937,745 (male: 2,148,348; female: 1,789,397) participants and followed them until December 2020 (mean follow-up 10.1 ± 1.3 years).
The average daily alcohol consumption was calculated using the drinking frequency (number of days per week) and the average amount consumed on each occasion. Information about frequency and amount of alcohol intake was acquired from the standardized self-reported questionnaire at enrollment. Then, to standardize the alcohol consumption, the amount was converted into grams of ethanol per day. Based on the ethanol consumption, alcohol drinking levels were divided into three categories; nondrinkers, mild drinkers, and heavy drinkers. The participants who drank less than 30 g/day of ethanol were categorized as mild drinkers, and those who drank over 30 g/day of ethanol were categorized as heavy drinkers.
Age, gender, low income, smoking, regular exercise, height, weight, waist circumference, body mass index, medical conditions including obesity, metabolic syndrome, chronic kidney disease, and laboratory results including fasting glucose, total cholesterol, high-density cholesterol (HDL), low-density cholesterol (LDL) and estimated glomerular filtration rate were the variables of this study.
Soft-tissue sarcoma was defined as ICD-10 codes C47 or C49 and the registration code for cancer (V193) with at least two outpatient or more than one inpatient claim per year.
Results: Among the 3,937,745 eligible participants, 969 were diagnosed with STS during the follow-up period, resulting in an incidence of 2.43 per 100,000 per person-year. Tables 1 and 2 present the baseline characteristics of male and female participants by drinking status.
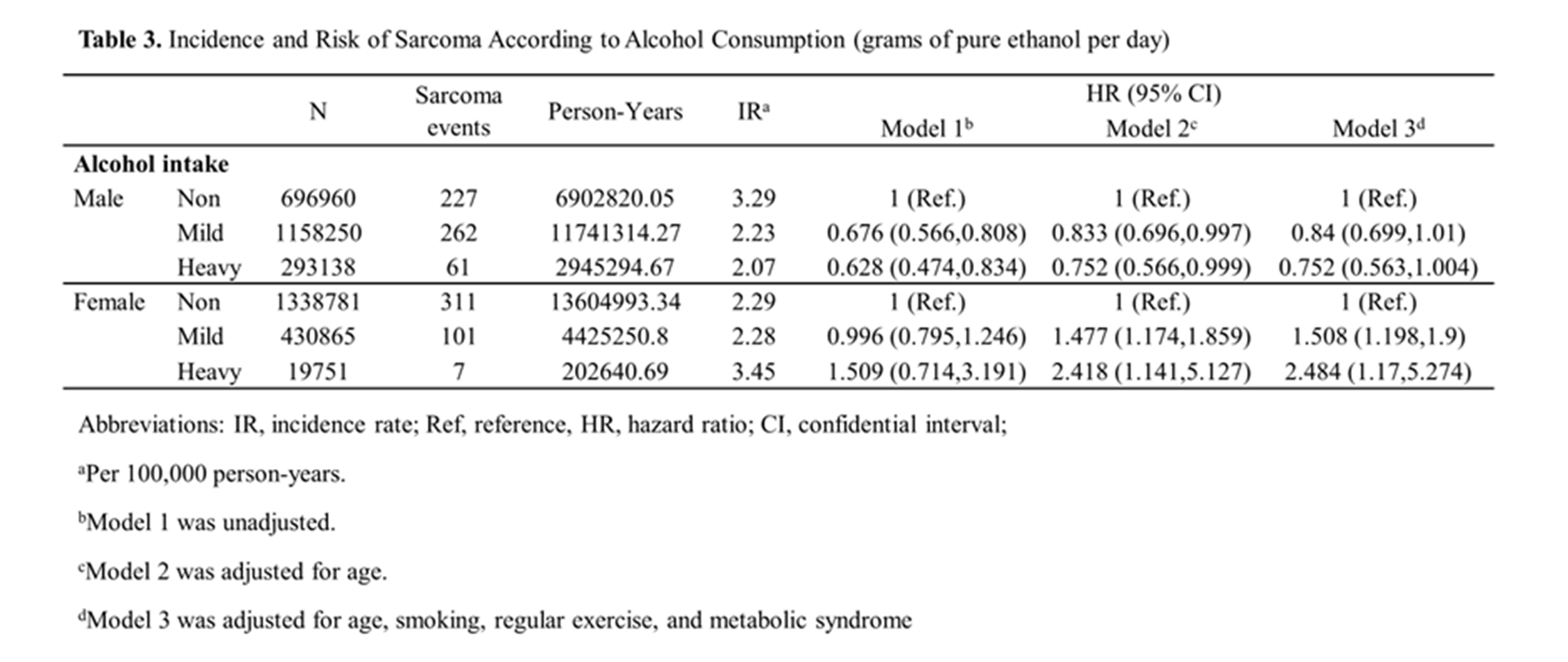
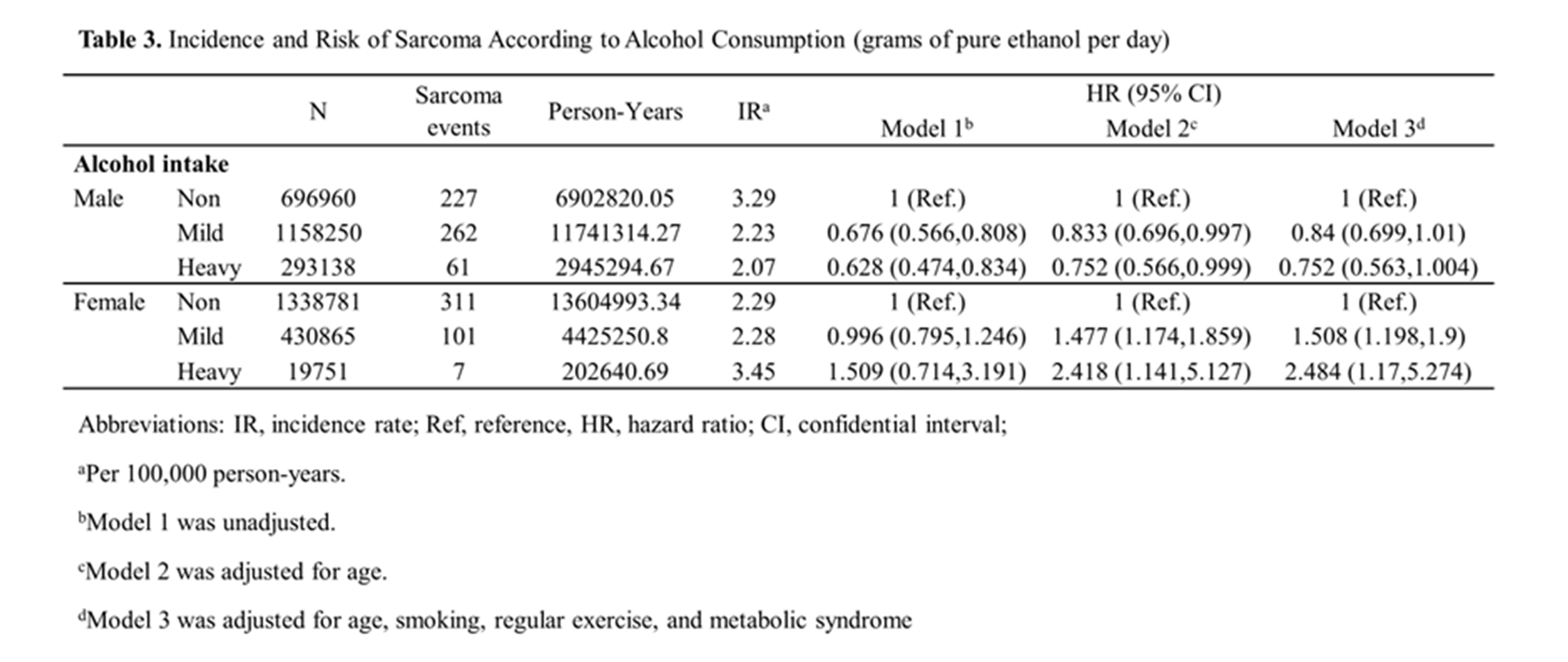
Among the 969 patients who were diagnosed with STS during the follow-up period of 10.1 ± 1.3 years, 550 were male and 419 were female. In the male group, compared with the nondrinkers (reference), the risk of STS among the drinkers was not significantly associated with mild and heavy drinking after the adjustment of covariates (adjusted HR [aHR], 0.84 [95% CI, 0.70 to 1.01] and aHR, 0.75 [95% CI, 0.56 to 1.00] respectively). However, in the female group, compared with nondrinkers (reference), the risk of STS among the drinkers was significantly associated with mild and heavy drinking after adjustment (aHR, 1.51 [95% CI, 1.20 to 1.90], and aHR 2.49 [95% CI, 1.17 to 5.27]) (Table 3).
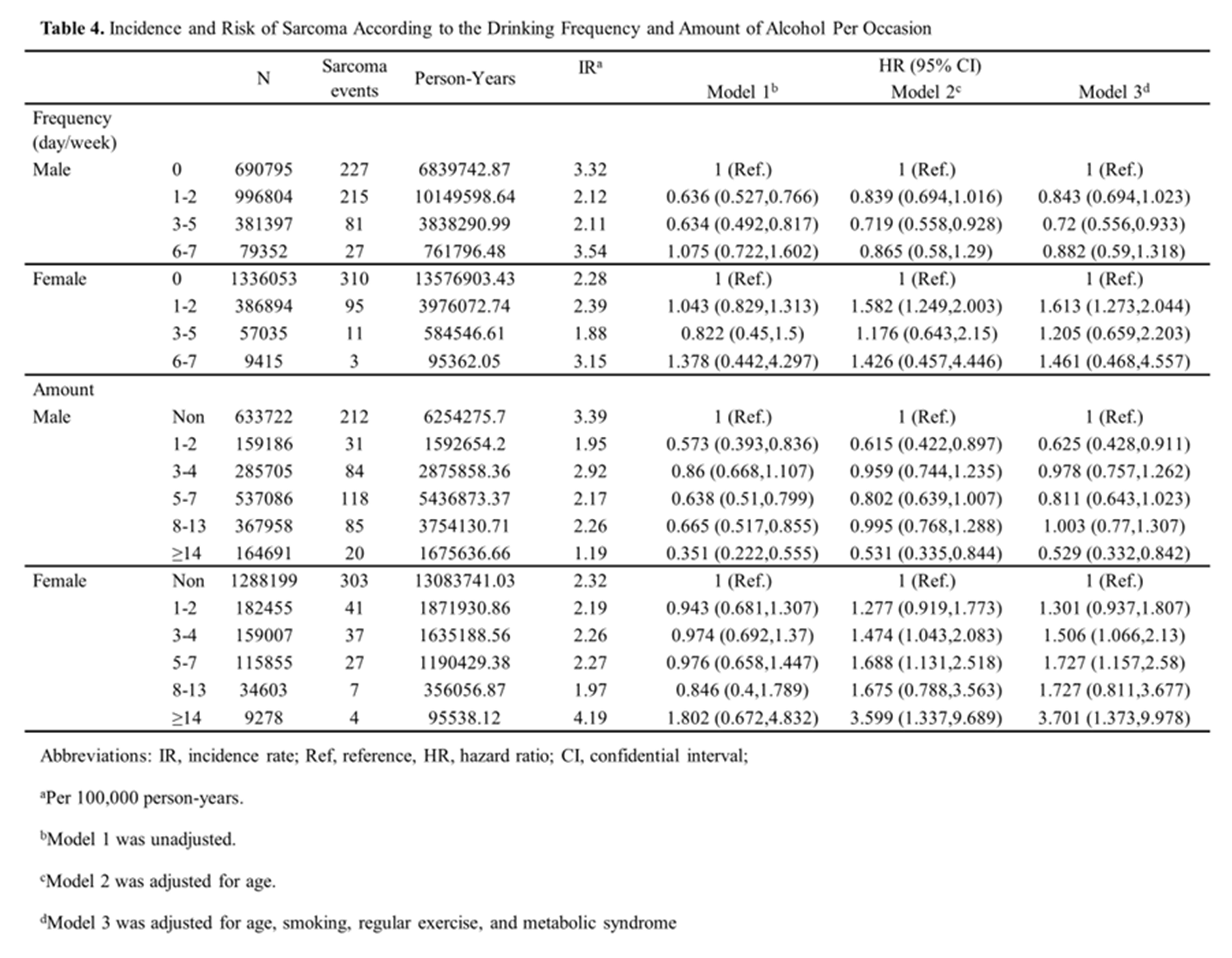
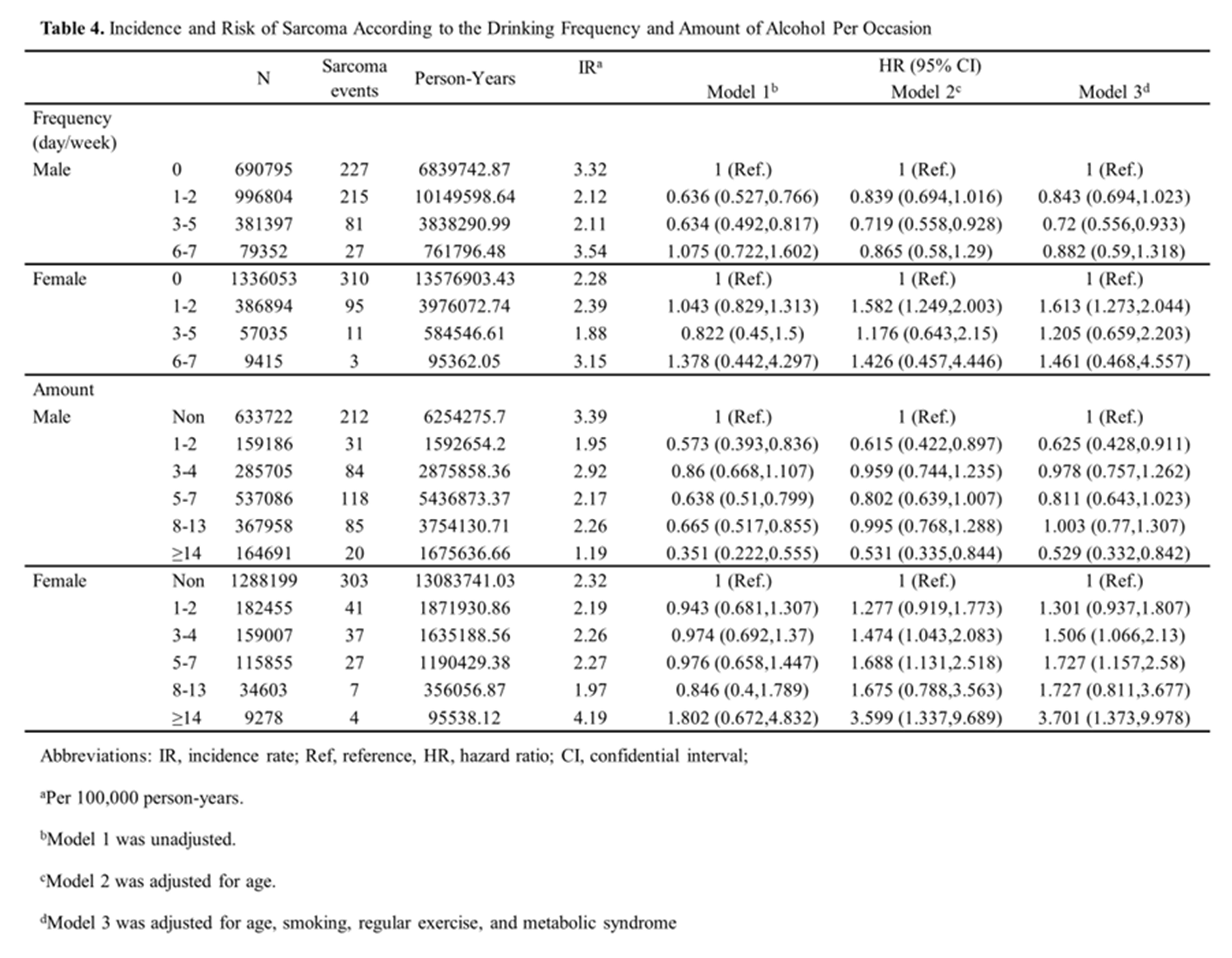
The STS risk, analyzed with drinking frequency and amount of alcohol consumption per occasion, is shown in Table 4. The frequency and amount of alcohol consumption were not significant risk factors in the male group. However, in the female group, drinking frequency of 1 to 2 days a week and amount of alcohol consumption of more than 14 glasses per occasion were both statistically significant risk factors for STS occurrence. In addition, the amount of alcohol consumption of more than 14 glasses per occasion (aHR 3.701 [95% CI, 1.38 to 9.98]) was a stronger risk factor than the drinking frequency of 6 to 7 days a week (aHR 1.46 [95% CI, 0.47 to 4.56]). While there was no significant difference in the hazard ratio based on drinking frequency, the hazard ratio increased with higher amount of alcohol consumption per occasion.
Conclusion: This research is the inaugural large-scale study to determine the association between graded increasing alcohol consumption and STS risk, and the difference in the risk among sexes. The nationwide population-based study demonstrated a statistically significant dose-response relationship between the level of alcohol consumption and the risk of STS among women. Therefore, we need proactive strategies to discourage alcohol consumption, which should be considered as a screening factor for STS.

Worldwide, alcohol consumption stands as a leading risk factor for oncogenesis and related deaths. Ethanol in alcoholic beverages and acetaldehyde, its major metabolite, are categorized as group 1 (carcinogenic to humans) by the International Agency for Research on Cancer. Nevertheless, global per-capita alcohol consumption has been increasing, and the upward trend poses a potential risk of escalating the overall burden of cancers. In particular, the Korea National Health and Nutrition Examination Survey reported that the prevalence of high-risk drinking, defined as the proportion of people aged ≥19 years who drink ≥2 times per week and consume a large amount of alcohol each time (an average of ≥7 glasses for male and ≥5 glasses for female per episode) was 3.4% in 2005 and 8.4% in 2018 among women, implying a pronounced rising trend.
Therefore, alcohol consumption might be a risk factor for STS. We conducted a population-based study using the nationwide claims data to explore the association between alcohol consumption and STS risk, and its differences between sexes, focusing on alcohol consumption and drinking frequency.
Methods: This was a retrospective population-based cohort study. Using the National Health Insurance Service (NHIS) database, which represents the South Korean population, we analyzed 4.2 million Korean adults aged 20 years of age and older. In South Korea, NHIS serves as a single health insurance provider to all Korean citizens and provides biannual regular free health checkups. This database includes demographic, socioeconomic, health checkups, and claims data of all insured Korean people. The checkup programs include data for medical history, family history, height, weight, waist circumference, blood pressure, laboratory tests, hearing and visual checkups. Also, in 2009, according to the activation of the Basic Act on Health Examination, social behavior surveys including smoking, alcohol consumption, and exercise were added. Therefore, we included individuals who underwent NHIS health checkups between January 2009, and December 2009, and tracked them until December 2020 to identify the incident of STS. The participation rate for NHIS health checkups in the index year 2009 was 67%.
We initially screened 4,234,415 participants who were aged 20 years and older and underwent health checkups in 2009. Among them, 286,384 individuals were excluded due to incomplete data, and 198 patients who were already diagnosed with STS before the index year were also excluded. In addition, to clarify causality, we excluded 10,088 participants who died or developed STS in the index year. Finally, we included 3,937,745 (male: 2,148,348; female: 1,789,397) participants and followed them until December 2020 (mean follow-up 10.1 ± 1.3 years).
The average daily alcohol consumption was calculated using the drinking frequency (number of days per week) and the average amount consumed on each occasion. Information about frequency and amount of alcohol intake was acquired from the standardized self-reported questionnaire at enrollment. Then, to standardize the alcohol consumption, the amount was converted into grams of ethanol per day. Based on the ethanol consumption, alcohol drinking levels were divided into three categories; nondrinkers, mild drinkers, and heavy drinkers. The participants who drank less than 30 g/day of ethanol were categorized as mild drinkers, and those who drank over 30 g/day of ethanol were categorized as heavy drinkers.
Age, gender, low income, smoking, regular exercise, height, weight, waist circumference, body mass index, medical conditions including obesity, metabolic syndrome, chronic kidney disease, and laboratory results including fasting glucose, total cholesterol, high-density cholesterol (HDL), low-density cholesterol (LDL) and estimated glomerular filtration rate were the variables of this study.
Soft-tissue sarcoma was defined as ICD-10 codes C47 or C49 and the registration code for cancer (V193) with at least two outpatient or more than one inpatient claim per year.
Results: Among the 3,937,745 eligible participants, 969 were diagnosed with STS during the follow-up period, resulting in an incidence of 2.43 per 100,000 per person-year. Tables 1 and 2 present the baseline characteristics of male and female participants by drinking status.
Among the 969 patients who were diagnosed with STS during the follow-up period of 10.1 ± 1.3 years, 550 were male and 419 were female. In the male group, compared with the nondrinkers (reference), the risk of STS among the drinkers was not significantly associated with mild and heavy drinking after the adjustment of covariates (adjusted HR [aHR], 0.84 [95% CI, 0.70 to 1.01] and aHR, 0.75 [95% CI, 0.56 to 1.00] respectively). However, in the female group, compared with nondrinkers (reference), the risk of STS among the drinkers was significantly associated with mild and heavy drinking after adjustment (aHR, 1.51 [95% CI, 1.20 to 1.90], and aHR 2.49 [95% CI, 1.17 to 5.27]) (Table 3).
The STS risk, analyzed with drinking frequency and amount of alcohol consumption per occasion, is shown in Table 4. The frequency and amount of alcohol consumption were not significant risk factors in the male group. However, in the female group, drinking frequency of 1 to 2 days a week and amount of alcohol consumption of more than 14 glasses per occasion were both statistically significant risk factors for STS occurrence. In addition, the amount of alcohol consumption of more than 14 glasses per occasion (aHR 3.701 [95% CI, 1.38 to 9.98]) was a stronger risk factor than the drinking frequency of 6 to 7 days a week (aHR 1.46 [95% CI, 0.47 to 4.56]). While there was no significant difference in the hazard ratio based on drinking frequency, the hazard ratio increased with higher amount of alcohol consumption per occasion.
Conclusion: This research is the inaugural large-scale study to determine the association between graded increasing alcohol consumption and STS risk, and the difference in the risk among sexes. The nationwide population-based study demonstrated a statistically significant dose-response relationship between the level of alcohol consumption and the risk of STS among women. Therefore, we need proactive strategies to discourage alcohol consumption, which should be considered as a screening factor for STS.